August 1, 2023- July 31, 2024
The NH Disability and Health Program (NH DHP) focuses on seven strategies the Centers for Disease Control and Prevention identified. This summary reports on the program activities for Year 3 of the current funding cycle (8/1/2023-7/31/2024) organized by strategy.




The DHAWG poses at the in-person June meeting in Concord, NH. From left to right: Megan Henly, Kris van Bergen-Buteau, Vanessa Blais, Robert Scholz, Kelly Ehrhart, Jennifer Pineo, Jennifer Fitzsimmons, Martha McLeod, Brittany Potvin, Cindy Lafond, Deb Ritcey, Emilia Poehlman, Kathy Bates, Toni Sumner-Beebe, Ashley Caswell, Karen Volle.
NH DHP Strengthens Oral Health Partnerships
ABLE NH, the state’s disability justice organization, identified oral healthcare access as a priority. The organization has taken a critical leadership role in improving access to oral healthcare for people with disabilities. ABLE NH facilitates a monthly Oral Healthcare Task Force where advocates and oral health stakeholders come together to discuss gaps and barriers and strategize around solutions. Since September 2023, NH DHP staff have attended this monthly meeting.
NH DHP’s participation in the task force has strengthened existing relationships and developed new partnerships with advocates and stakeholders. Additionally, NH DHP staff identified an area where the program could address barriers to accessible oral healthcare for people with disabilities: training oral healthcare professionals in disability-competent care. Through the NH DHP partnership network, our team identified a content area expert in oral health and four disability advocates with lived experience to contribute to a new Responsive Practice module, which is already in production.
Partnership Spotlight: Granite YMCA
In August 2023, NH DHP was awarded new funding from the National Center on Health, Physical Activity and Disability (NCHPAD) to implement the NCHPAD inclusive Community Implementation Process (NiCIP) in collaboration with the Granite YMCA. This process supports Granite YMCA in identifying inclusion gaps and solutions within their organization. An Inclusive Health Coalition guides this process, which is made up of internal and external stakeholders. NH DHP has developed new partnerships and enhanced previous ones through this coalition. NH DHP hopes to leverage this work to pursue sustainable change within the Granite YMCA. Future change can potentially increase access to health and wellness opportunities for people with disabilities in the communities the Granite YMCA serves.


What is a milestone? Progress toward addressing barriers, gaps, and needs as acknowledged in the 2022 health and wellness needs assessments. This groundwork, ideally, should lead to meaningful, sustainable Policy, System, and Environmental changes.
NH DHP LEND Trainee Focuses on Food Security
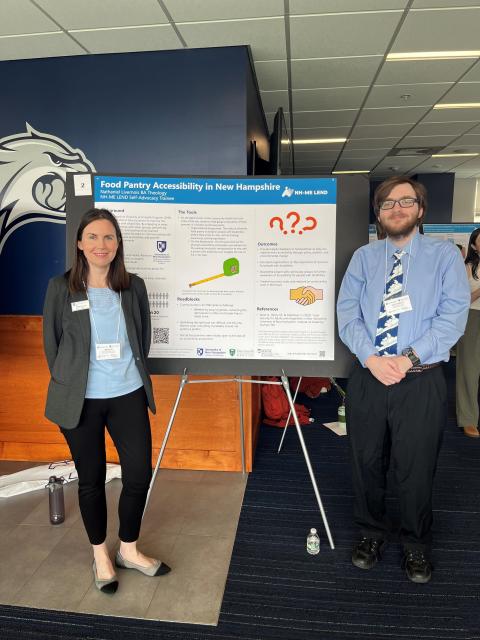
Megan Henly and Nathaniel Livernois at the LEND Capstone event in May 2024.
Through feedback from the DHAWG and the needs assessments, DHP identified food security as a significant health issue for people with disabilities in NH. This year, DHP published a Food Security & Disability Needs Assessment Report. Nathaniel Livernois, a student in the NH-ME Leadership Education in Neurodevelopmental Disabilities (LEND) program, worked with the DHP team to conduct accessibility assessments of food pantries in his NH community as part of his leadership placement. Nathaniel used the National Center for Health, Physical Activity, and Disability’s (NCHPAD) Community Health Inclusion Index to assess for organizational and environmental barriers that could limit access to food for people with disabilities. Through his LEND leadership placement, Nathaniel assessed four pantries in the Greater Derry, New Hampshire area. In July 2024, Nathaniel joined NH DHP as a staff member to continue this work in Year 4.
Spotlight: PATH Program
NEP PATH Program Continues To Make Positive Impact
NH DHP is pleased to have partnered with Northeast Passage (NEP) for a second year to evaluate factors and strategies impacting health equity for adults with mobility limitations in New Hampshire. NEP’s community-based recreational therapy model, designed to improve access to home and community environments, is instrumental in promoting long-term health outcomes. Participants met with an NEP Recreational Therapist to develop a plan for enhancing health and well-being, with the therapist conducting a comprehensive evaluation using both standardized assessment tools and a strengths-based interview. This process included setting and revisiting goals at the beginning of services and discharge.
Key health measures evaluated included happiness, quality of life, functioning, and pain interference. Comparisons of pre- and post-service scores demonstrated progress in these areas, aligning with previous research on this program’s effectiveness. In the discharge survey, participants frequently identified their top three areas of impact as: “Confidence in my ability to engage in activities that support my health,” “more positive experiences and feelings in my day-to-day life,” and a “sense of achievement or purpose through engaged living.”
12 Individuals served

Healthcare Provider Training
Administer and evaluate a training for healthcare providers on accessible preventive health care


UNH Nursing and NH DHP collaborate on Responsive Practice outreach video
In Year 3, two professors from the University of New Hampshire (UNH) nursing program implemented policy changes to their course syllabi, requiring that their students complete Responsive Practice as part of the curricula. Because this course is mandatory for all nursing students, all future UNH Nursing students will receive training in providing disability-competent care and screening.
This change reflects a commitment to enhancing disability competence among nursing students. NH DHP heard from UNH Nursing faculty and students about the importance and value of including disability competence training in health education programs through the brief clip below. NH DHP plans to use this video as an outreach tool to encourage faculty from other health education programs to adopt similar practices. The UNH Nursing program is an excellent example of integrating disability competence training into existing curricula. We hope this inspires other programs statewide to follow their lead and educate future health professionals on best practices when working with patients with disabilities.
Linkage Project
Implement and evaluate a demonstration project to link adults with IDD to preventive health care and health promotion programs in their community


New Partnership with NH Special Olympics to Share the Health Linkage Program
This year, NH DHP established a new partnership with Special Olympics-New Hampshire (SONH), creating a valuable opportunity to introduce the Health Linkage Program to SONH athletes. Health Linkage Program staff attended the SONH Winter Games in March, where they shared information with athletes and their families. SONH then invited the team back to participate in their Healthy Athletes event at the statewide summer games in June. Athletes who received referrals from their health exams or wanted to work on a health goal scheduled informational calls and appointments with our Linkage Coordinators onsite.

Living Well in the Community incorporated into UNH-Bridges Curriculum
NH DHP worked with the UNH Bridges Training Series, a UNH Institute on Disability program that offers college and career training for young adults ages 18-24 with intellectual disabilities (ID). Bridges Training staff incorporated the Living Well training into the existing curriculum on healthy and social aspects of life. Four participants completed the training through their enrollment in the Bridges program.
After this successful Living Well session, DHP staff solicited feedback from our two program hosts to date: the UNH Bridges Program and Granite State Independent Living. Our team also received feedback from prospective partners at the Granite YMCA who were trained as Living Well facilitators. DHP incorporated input received in these feedback sessions by updating the training materials in consultation with the authors. In response, NH DHP staff drafted new slides incorporating plain language and more inclusive imagery to support future workshops in Years 4 and 5.
NH DHP Continues Progress in Three Focus Areas in Year 3
PSE changes result from the relationship between our partnerships and needs assessments, conducted within an evaluation of our resources and partners' resources. We continue to be committed to three topical areas identified as important to our advisory work group and our partners: food security and nutrition, transportation, and oral health. As our program activities above demonstrate, we have met milestones that we anticipate will be the pathways to lasting PSE changes.
Food Security and Nutrition: We continue to reach out to local food pantries to provide them with assessments to understand how they could improve accessibility to their patrons. We anticipate this will result in new relationships with individual sites and could also yield findings useful to other local food and nutrition programs.
Transportation: NH DHP continues to be represented on regional transportation boards. In addition, our team hosts a disability transportation work group that brings together advocates and program representatives from other UNH programs and regional organizations focusing on disability or transportation.
Oral Health: This year, our team spent time considering how we could leverage our resources as trainers in providing disability-competent, responsive healthcare to dental providers so that we may improve access to quality oral healthcare for adults with disabilities in NH. This is particularly timely as the adult Medicaid benefit expanded to include dental benefits in 2023. This work continues.
NH DHP Brings Disability Lens to Local Health Conferences
This spring, the NH DHP presented about disability and accessibility to healthcare workers at two local conferences. Megan Henly and Kathy Bates, DHP’s Accessibility and Inclusion Specialist, delivered “Lighting the Way to Inclusive Health for the Disability Community” to community health workers at the NH Community Health Worker Summit and “Identifying Barriers to Substance Misuse Treatment” to substance use workers at the Strafford County Public Health Network (SCPHN) Addiction Summit. Both presentations were well-received, with attendees appreciating the blend of Kathy’s lived experiences and Megan’s data-driven insights. One participant from the CHW Summit noted, “I liked the first-hand experience from Kathy. Megan’s presentation of statistics put the numbers into perspective as well.” Through these efforts, NH DHP aims to leverage opportunities to educate health professionals about disability inclusion to identify sustainable organizational changes that will improve the lives of people with disabilities across the state. An attendee at the SCPHN shared that one thing they will do differently after the training is “ensure that our residential program can be more accessible as it's in an old house.”
Looking Ahead
Year 4 goals, objectives, and partnerships
- Partnerships: NH DHP identified an opportunity to include additional voices in the DHAWG and plans to recruit additional individuals to the advisory board to ensure diverse perspectives are included.
- Needs Assessment: NH DHP will utilize the NCHPAD Community Health Inclusion Index to support food security organizations as they assess their organizations and environments for accessibility and inclusion. NH DHP will also continue to support Northeast Passage’s PATH program, which has proven to be impactful in bridging the gap in unmet health needs for adults with mobility limitations.
- Healthcare Provider Training: NH DHP will continue to conduct outreach to health professional education programs to encourage faculty to incorporate Responsive Practice into their curriculum. NH DHP will also identify additional events and opportunities to market to NH-based healthcare providers.
- Linkage: The NH Linkage Team, in collaboration with the NH DHP team, will implement an updated outreach plan that includes site visits to area agencies across the state. The team hopes to create meaningful relationships with case managers to refer adults with unmet health needs to the program.
- Evidence-Based Intervention: Granite YMCA has trained two Community Health Workers as Living Well in the Community (LWIC) facilitators and plans to host at least two workshops in Year 4.
- PSE: NH DHP will continue the coalition building conducted in Years 2 and 3 to encourage PSE changes in oral health, food security/nutrition, and transportation. One area of potential PSE change includes environmental or systemic changes within food pantries assessed by NH DHP using the NCHPAD tools. Additional opportunities for PSE changes within other partner organizations may present throughout the year.
- Dissemination: NH DHP plans to identify local conferences to offer training opportunities for health professionals. NH DHP hopes that by educating healthcare workers about disability, accessibility, and inclusion, they will apply what they’ve learned to create organizational change.
Acknowledgements
This publication was supported by cooperative agreement number DD000025 with the U.S. Centers for Disease Control and Prevention (CDC). Its contents are solely the authors' responsibility and do not necessarily represent the views of CDC.
The program staff at the University of New Hampshire Institute on Disability (UNH IOD) gratefully acknowledge the many individuals, families, advocates, agencies, and organizations whose work has paved the way for current public health efforts, programs, and initiatives.
This summary was prepared by Megan Henly, PhD, and Emilia Poehlman, MSW, at the UNH IOD. Thanks to DHP’s Kathy Bates, Hannah Pease, Toni Sumner-Beebe, Karen Volle, Holly Magowan, and Nathaniel Livernois for their input and contributions toward program activities. Design and website support were provided by Kate Filanoski. Thanks also to the Disability and Health Advisory Work Group who were active in Year 3:
Alternative formats of this summary are available. Please contact disability.health@unh.edu to request an alternative format.
- Emily Bird, NH Division of Public Health Services
- Carol Conforti-Adams, Sunset Hill Education Institute
- Kelly Ehrhart, Disability Advocate
- John Fenley, Disability Advocate
- Joshua Gehling, NH Bureau of Developmental Services
- Whitney Hammond, NH Division of Public Health Services
- Cindy Lafond, Granite YMCA
- Kelly Main, NH Bureau of Developmental Services
- Jennifer McLaren, MD, Dartmouth-Hitchcock
- Martha McLeod, New Futures / New Hampshire Alliance for Healthy Aging
- Jennifer Pineo, NH Family Voices
- Lisa Plotnik, MD, Dartmouth-Hitchcock
- Brittany Potvin, Disability Advocate
- Laura Remick, North Country Health Consortium
- Deb Ritcey, MPA/HA, Granite State Independent Living
- Isadora Rodriguez-Legendre, MSW, NH Council on Developmental Disabilities
- Bob Scholz, MS, LMHC, Center for START Services
- Valarie Tetreault, MAPP, Community Bridges

